Antibiotics kill bacteria by targeting their essential structures and processes. They may weaken the cell wall, causing bacteria to burst during growth, or disrupt the cell membrane to allow harmful substances to leak in. Many block protein synthesis, preventing bacteria from making crucial proteins. Others stop DNA or RNA production, halting reproduction. Understanding these mechanisms reveals how antibiotics selectively attack bacteria while sparing human cells—if you keep exploring, you’ll discover even more fascinating details.
Key Takeaways
- Antibiotics target bacterial cell structures like the cell wall and membrane, causing weakening, rupture, or increased permeability leading to bacterial death.
- They inhibit bacterial protein synthesis by binding to ribosomes, blocking growth and causing cell death.
- Many antibiotics interfere with bacterial DNA and RNA synthesis, preventing replication and transcription necessary for bacterial proliferation.
- They disrupt essential bacterial enzymes and metabolic pathways, such as folic acid synthesis, which are absent in human cells.
- Antibiotics are selective, targeting bacterial-specific components while sparing human cells, minimizing side effects.
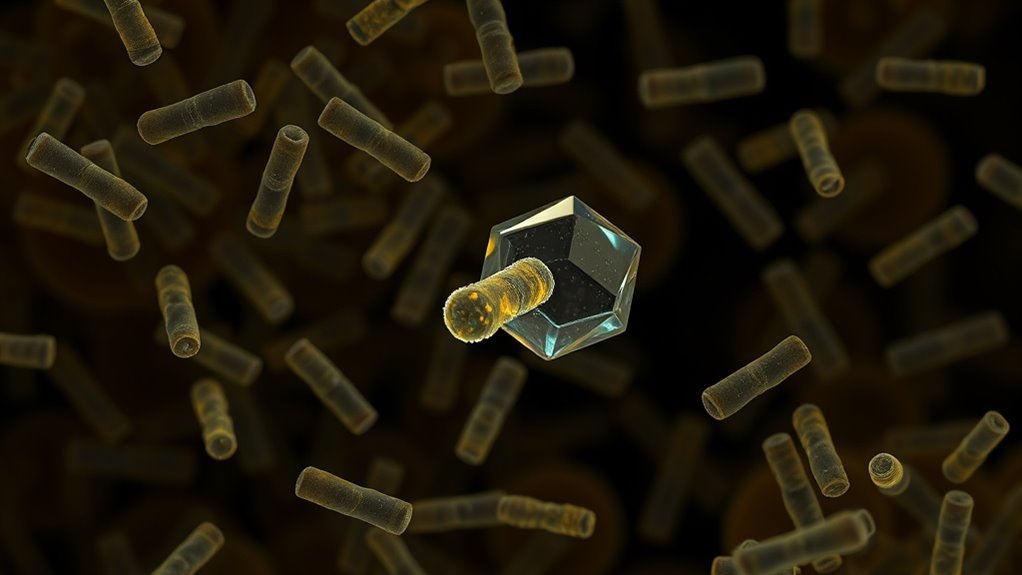
Disrupting Bacterial Cell Wall Formation

Antibiotics that target bacterial cell wall formation work by disrupting the synthesis of peptidoglycan, an essential component that gives bacteria their structural strength. You’ll find that β-lactams, such as penicillin and cephalosporins, inhibit enzymes responsible for building the peptidoglycan layer. Peptidoglycan is a key component of bacterial cell walls, providing structural integrity. Glycopeptides like vancomycin block the cross-linking process, weakening the wall further. Carbapenems and monobactams also interfere with cell wall synthesis, while D-cycloserine hampers peptidoglycan precursor production. These antibiotics work by preventing the bacteria from maintaining their structural integrity, causing holes to form in the cell wall. As the wall weakens, the bacteria become vulnerable to lysis during growth, leading to their death. Because mammalian cells lack a cell wall, these drugs selectively target bacteria. Additionally, understanding the mechanism of action helps in developing new antibiotics to combat resistant strains.
Inhibiting Protein Production in Bacteria
Bacterial protein production is essential for growth and survival, occurring on the 70S ribosome composed of the 30S and 50S subunits. Antibiotics target specific steps in this process, such as the formation of the 30S initiation complex, assembly of the 70S ribosome, and elongation of the polypeptide chain. Tetracyclines bind reversibly to the 30S subunit, blocking aminoacyl-tRNA from attaching to the A site, which halts translation initiation. Aminoglycosides irreversibly bind to the 30S subunit, causing misreading of mRNA and producing faulty proteins. They also disrupt bacterial membrane functions, further contributing to their bactericidal activity. Macrolides, chloramphenicol, and streptogramins target the 50S subunit, disrupting elongation and peptide bond formation. These drugs interfere with bacterial protein synthesis, effectively stopping bacterial growth or killing the bacteria outright. Understanding the mechanisms of action helps in developing more effective antimicrobial agents and combatting resistance.
Blocking Bacterial DNA and RNA Synthesis

Blocking bacterial DNA and RNA synthesis is a crucial strategy in antibiotic therapy. Quinolones like ciprofloxacin target DNA gyrase, an enzyme essential for managing DNA supercoiling during replication. By inhibiting DNA gyrase, these drugs prevent bacteria from copying their genetic material, leading to cell death. DNA Gyrase is vital for maintaining the negative supercoiling necessary for bacterial DNA replication and transcription. Metronidazole causes DNA fragmentation by inducing damage inside anaerobic bacteria and parasites, disrupting their genomes. Rifampin binds to bacterial RNA polymerase’s β subunit, halting transcription initiation and stopping protein production. Actinomycin D also inhibits transcription but does so by binding directly to DNA, distorting its structure. These mechanisms effectively shut down bacterial gene expression, preventing growth and reproduction. Since they target bacterial enzymes and DNA, they minimize harm to human cells, making them essential tools in fighting bacterial infections.
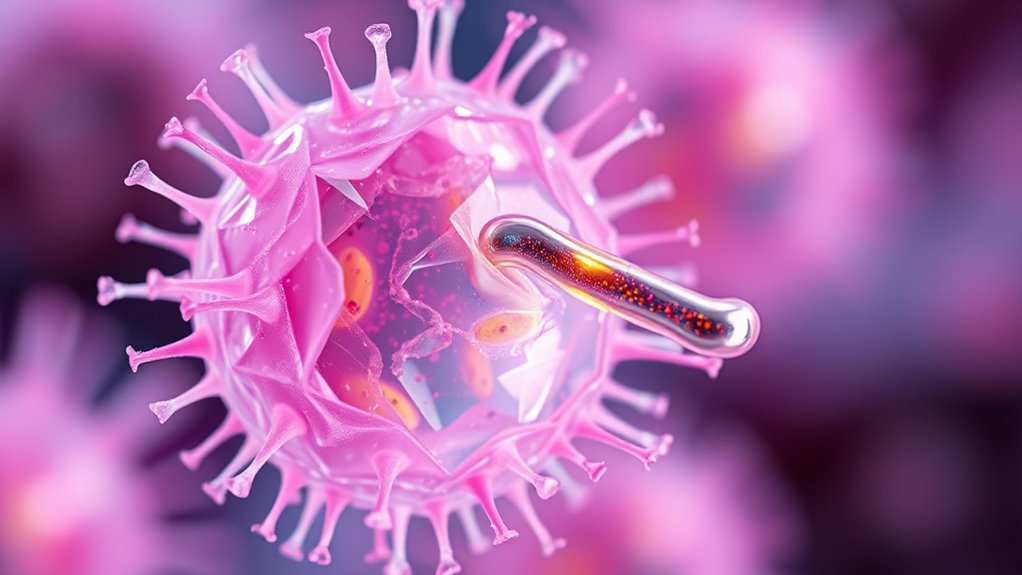
Increasing Bacterial Cell Membrane Permeability

Disrupting this barrier can help antibiotics reach their targets more effectively. Polymyxins, for example, bind to lipopolysaccharides (LPS), destabilizing the membrane. Other compounds can modify porin function or alter membrane lipids to increase permeability. Variations in LPS structure and porin expression can significantly influence the permeability barrier, affecting antibiotic susceptibility. Additionally, understanding the offensive security strategies used by antibiotics can aid in designing more effective drugs. When these strategies succeed, antibiotics penetrate more easily, reaching intracellular targets and disrupting *vital* processes. Increased permeability also causes leakage of bacterial components, leading to cell death.
Targeting Bacterial Enzymes for DNA Replication

Targeting enzymes involved in DNA replication is an essential strategy in the development of antibiotics. Quinolone antibiotics attack bacterial DNA gyrase and topoisomerase IV, which are indispensable for DNA topology and replication. These drugs form stable complexes with the enzymes and DNA, preventing religation and causing double-stranded breaks that kill bacteria.
By inhibiting DNA gyrase, which introduces negative supercoils, and topoisomerase IV, which decatenates replicated chromosomes, they disrupt critical processes. Resistance may develop through mutations in the enzyme genes, reducing drug binding.
Additionally, rifampicin targets bacterial RNA polymerase, blocking transcription and indirectly causing DNA damage. This approach selectively affects bacteria, sparing human cells, and effectively halts bacterial proliferation by interfering with key enzymes in DNA replication.
Overcoming Bacterial Resistance Strategies
As bacteria develop resistance to antibiotics, it becomes increasingly important to implement strategies that counteract these defenses. You can do this through infection prevention, using adjuvants, developing new drugs, phage therapy, and improving diagnostics. Infection control practices, like hand hygiene and rapid diagnosis, limit resistant bacteria spread. Antibiotic adjuvants enhance existing drugs, inhibit resistance enzymes, and disrupt biofilms. Novel approaches, including antimicrobial peptides, nanomaterials, and CRISPR, target resistance genes directly. Phage therapy offers a precise, bacteria-specific alternative that reduces resistance pressure. Improving diagnostics allows targeted treatment, reducing unnecessary antibiotic use. Antibiotic resistance is a growing global concern, making these strategies vital in the fight against resistant infections. Additionally, ongoing research into Kia Tuning technologies inspires innovative methods to optimize treatment delivery and efficacy. Here’s a visual overview:
| Strategy | Action | Benefit |
|---|---|---|
| Infection Prevention | Hand hygiene, rapid diagnosis | Limits spread of resistance |
| Antibiotic Adjuvants | Inhibit enzymes, disrupt biofilms | Restores antibiotic effectiveness |
| Novel Drug Design | Use peptides, nanomaterials | Bypass resistance mechanisms |
| Phage Therapy | Use bacteriophages | Target resistant bacteria specifically |
How Antibiotics Selectively Kill Bacteria
Antibiotics achieve their bacteria-killing effects by exploiting fundamental differences between bacterial cells and human tissues. You can target structures like peptidoglycan in bacterial cell walls, which human cells lack, making drugs like β-lactams highly specific. Additionally, many antibiotics are designed to target bacterial cell wall synthesis, a process absent in human cells. Similarly, bacterial ribosomes differ from human 80S ribosomes, allowing antibiotics such as tetracyclines and macrolides to inhibit bacterial protein synthesis without harming human cells. Enzymes involved in bacterial DNA replication, like DNA gyrase, are distinct from their human counterparts, so drugs like quinolones selectively block bacterial DNA processes. Ultimately, some antibiotics interfere with bacterial-specific metabolic pathways, such as folic acid synthesis, which humans don’t perform. These differences enable antibiotics to effectively kill bacteria while minimizing damage to your tissues.
Frequently Asked Questions
How Do Antibiotics Distinguish Between Bacterial and Human Cells?
You might wonder how antibiotics tell bacteria apart from human cells. They target structural differences, like bacterial cell walls made of peptidoglycan, which human cells lack.
They also bind to bacterial ribosomes—30S and 50S subunits—different from human ribosomes, preventing protein synthesis in bacteria.
Additionally, antibiotics interfere with bacterial enzymes and pathways absent in humans, ensuring they attack bacteria without harming your own cells.
Can Antibiotics Target Viruses or Fungal Infections?
It’s amusing how some believe antibiotics might target viruses or fungi—they’re just not built for that. Viruses lack the structures antibiotics attack, like cell walls, and fungi have different cell components.
So, you’d need different medicines—antivirals for viruses and antifungals for fungi. Using antibiotics here isn’t just pointless; it can cause harm, resistance, and delay proper treatment.
Always get the right diagnosis before choosing your medicine.
What Causes Bacteria to Develop Resistance to Antibiotics?
You might wonder what causes bacteria to develop resistance to antibiotics. It happens when bacteria undergo spontaneous mutations or acquire resistance genes through horizontal gene transfer.
When exposed to antibiotics, resistant bacteria survive and multiply, especially if antibiotics are overused or misused.
Poor infection control, environmental contamination, and inadequate diagnostics also promote resistance by giving bacteria more opportunities to adapt and spread resistant traits.
Are All Antibiotics Equally Effective Against Gram-Positive and Gram-Negative Bacteria?
Think of antibiotics as keys and bacteria as locked doors. Not all keys open every door.
You find that some keys fit easily into the lock of Gram-positive bacteria, but struggle with the complex, guarded doors of Gram-negative bacteria.
How Do Combination Therapies Improve Antibiotic Effectiveness?
You want to know how combination therapies improve antibiotic effectiveness. By using multiple drugs, you target different bacterial pathways simultaneously, making it harder for bacteria to survive.
This enhances the overall killing power, often creating synergistic effects. Plus, it helps slow resistance development by requiring bacteria to undergo multiple mutations.
As a result, combination therapies can be more effective than single antibiotics, especially against resistant infections.
Conclusion
Now that you know how antibiotics work to kill bacteria, it’s clear they target essential processes like cell wall formation and DNA replication. But do you realize how vital it is to use them responsibly to prevent resistance? If bacteria keep evolving, will antibiotics remain effective? Staying informed and cautious with antibiotic use ensures these powerful drugs continue to save lives. After all, isn’t protecting your health worth understanding how these medicines fight infections?