Rapid antigen tests detect specific viral proteins in respiratory samples like nasal swabs by using antibodies that bind to these proteins, creating a visible signal. They provide quick results—usually within 15 to 30 minutes—and are easy to use at point-of-care settings. While highly specific, their sensitivity varies depending on viral load and test quality. Understanding how these tests work explains their benefits and limitations, and if you keep exploring, you’ll learn more about their role in healthcare.
Key Takeaways
- Rapid antigen tests detect specific viral proteins, such as nucleocapsid or envelope proteins, from respiratory samples.
- They use antibodies conjugated to colloidal gold or fluorescence to bind and visually reveal viral antigens.
- Sample collection (nasal or nasopharyngeal swabs) and proper handling are critical for accurate detection.
- Sensitivity depends on viral load; higher loads yield more reliable results, while lower loads increase false negatives.
- These tests offer quick, point-of-care results, enabling timely clinical decisions and public health interventions.
How Rapid Antigen Tests Detect Viral Proteins in Respiratory Samples

Rapid antigen tests detect viral proteins by targeting specific structural components present in respiratory samples. You typically collect samples via nasal or nasopharyngeal swabs, which capture mucosal viral particles.
When you immerse the swab in an extraction buffer, it disrupts the viral membrane, releasing proteins like nucleocapsid (NP), envelope, or fusion proteins. These proteins are chosen because they’re abundant and conserved across viral strains, making them reliable markers.
The test employs antibodies that specifically bind these proteins. In a lateral flow device, conjugated antibodies labeled with colloidal gold or fluorescence attach to the viral proteins. As the sample flows, antigen-antibody complexes are captured at the test line, producing a visible signal that indicates the presence of the virus.
The Speed and Simplicity of Rapid Diagnostic Testing

The speed and simplicity of rapid diagnostic tests allow healthcare providers to quickly identify influenza and RSV infections, often delivering results in just 15 minutes to an hour. This rapid turnaround enables you to make timely clinical decisions, such as starting antiviral treatments or implementing infection control measures. Many of these tests utilize AI-driven technologies to streamline processing and improve accuracy. Advanced tests, like the Xpert® Xpress, can deliver results in around 25 minutes while maintaining high accuracy. These tests use straightforward sample collection methods, typically nasal or nasopharyngeal swabs, which are minimally invasive and easy to handle. Most rely on simple immunoassay formats that require little training or equipment, making them suitable for point-of-care settings. This combination of speed and simplicity allows for efficient testing even in resource-limited environments or during peak respiratory virus seasons.
Understanding Sensitivity and Specificity in RAT Performance

Understanding how well rapid antigen tests (RATs) detect influenza and RSV requires examining their sensitivity and specificity. Sensitivity indicates how accurately the tests identify infected individuals.
For influenza A, sensitivity ranges from 68% to 85% at high viral loads (Ct <25). RSV sensitivity varies widely, from 40% to 100%, depending on the RAT brand and viral load, with an overall pooled sensitivity around 80%. Sensitivity drops as viral loads decrease.
High viral loads are critical for accurate detection, and tests tend to perform better when viral concentrations are elevated. Emerging technologies in diagnostic testing, such as digital readouts and AI-assisted analysis, are expected to enhance accuracy further.
Specificity reflects the test’s ability to correctly identify uninfected individuals, which is generally high—around 97% for RSV and above 95% for influenza—resulting in few false positives. High specificity makes RATs reliable for confirming positive cases, especially during outbreaks.
High specificity means RATs reliably confirm true positives during outbreaks.
However, sensitivity depends on viral load, patient age, and symptom duration, affecting overall accuracy. Integrating AI in medical diagnostics is expected to improve the precision of rapid testing methods in the future.
Factors Influencing Test Accuracy and Reliability

Various factors influence the accuracy and reliability of rapid antigen tests for flu and RSV, with both technical and procedural elements playing critical roles. Analytical sensitivity depends on the antibody-antigen binding affinity, which varies by manufacturer and affects detection thresholds. Viral load in the sample is essential—higher loads improve sensitivity, while lower loads may cause false negatives.
The assay’s design, including antibody selection and epitope targeting, impacts binding efficiency. Sample collection quality is important; improper technique or delays can degrade antigens, reducing accuracy. Patient factors like symptom timing and severity influence viral shedding, affecting detection. Additionally, proper sample handling procedures are crucial to preserve antigen integrity and prevent false results.
Environmental conditions, operator training, and storage also matter—temperature, humidity, and batch consistency can alter test performance. Adhering to proper procedures ensures more consistent, reliable results. Furthermore, incorporating remote testing options can enhance access and reduce variability in testing environments.
Furthermore, ongoing advancements in test technology aim to improve sensitivity and reduce false negatives, making these tests more reliable in various settings.
Clinical Applications and Benefits of Rapid Antigen Testing
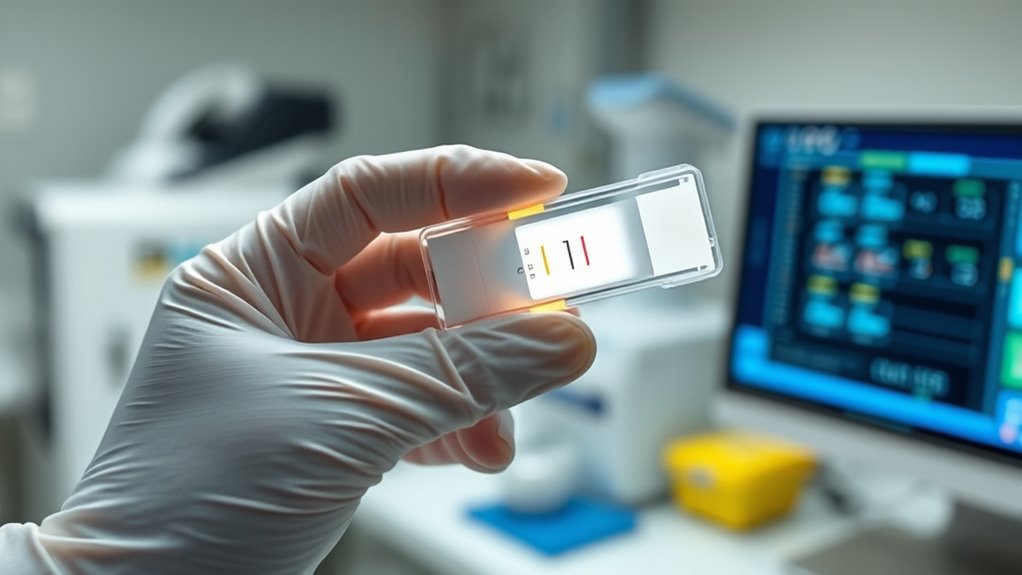
Rapid antigen tests are widely valued in clinical settings because they deliver quick results, often within an hour, making them ideal for point-of-care use. Their speed and convenience allow you to make immediate decisions, especially in emergency departments or community clinics.
These tests are cost-effective, offering a low-cost alternative to molecular methods like PCR, and can be performed outside traditional labs, increasing accessibility. They’re especially useful for high-risk groups, such as the elderly and children, enabling rapid outbreak management.
Their high specificity ensures reliable positive results, supporting targeted treatments and reducing unnecessary isolation. By providing quick, accurate diagnoses, rapid antigen tests help you initiate timely interventions, improve patient outcomes, and support effective infection control measures in diverse healthcare settings. Proper test administration is essential to ensure accurate and reliable results.
Limitations and Challenges in Detecting Flu and RSV

While rapid antigen tests offer quick results, their ability to accurately detect flu and RSV faces significant limitations. Sensitivity varies widely: RSV tests are more reliable (75-88%) than influenza RIDTs (50-70%), but performance drops in adults, with RSV sensitivity falling to just 29%. Influenza B is also less detectable than influenza A.
During peak activity, false negatives increase, risking missed diagnoses. Specificity is generally high (95-99%), yet false positives can occur, especially in low-prevalence periods. Sample quality and timing critically affect accuracy, with early testing yielding better results.
Device type matters: analyzer-based tests improve sensitivity. However, limitations like strain detection gaps, variability across populations, and dependence on proper sample collection hinder consistent reliability, emphasizing the need for confirmatory testing in many cases.
The Role of RATs in Public Health and Patient Care

Have you ever wondered how rapid antigen tests (RATs) shape public health and patient care? These tests quickly identify most infectious cases, helping control outbreaks through early detection, even if they’re less sensitive than PCR tests.
Designed for screening, RATs detect viral loads that indicate contagiousness, offering results in just 15-30 minutes. This rapid turnaround supports swift decision-making, especially in community settings or healthcare facilities, aiding triage and reducing hospital strain.
RATs also help differentiate infectious from non-infectious patients, guiding treatment and isolation. Their ease of use and quick results enable large-scale screening in schools, workplaces, and public spaces, reducing transmission.
Frequently Asked Questions
How Do Different Brands of RATS Compare in Accuracy?
You want to know how different brands of rapid antigen tests compare in accuracy. Some brands, like SD Biosensor STANDARD Q, perform better with higher sensitivity, correctly identifying positive cases around 88%.
Others, like BinaxNOW, have lower sensitivity but maintain high specificity. The choice depends on your needs, but generally, brands vary in accuracy, especially in detecting low viral loads or asymptomatic cases.
Can Rapid Tests Distinguish Between Flu and RSV Infections?
You’re asking if rapid tests can tell the difference between flu and RSV infections. Yes, they can.
These tests use specific antibodies on the strip to identify unique viral proteins, allowing you to see which virus is present within 15 to 30 minutes.
This distinction helps healthcare providers quickly decide on treatment, but remember, false negatives can occur, so confirmatory tests might still be necessary if symptoms persist.
What Are the Effects of Sample Collection Timing on RAT Results?
Did you know that collecting samples early in illness can boost RAT sensitivity by up to 30%? The timing of sample collection directly influences test accuracy.
If you collect too late, viral loads drop, increasing false negatives. You should aim to test within the first few days of symptoms for the best results.
Consistent timing ensures reliable outcomes, reducing the chance of misdiagnosis and enabling quicker treatment decisions.
Are There Any New Advancements Improving RAT Sensitivity?
You’ll find that recent advancements are considerably improving RAT sensitivity. Researchers are developing multiplex tests to detect multiple viruses simultaneously, while new biosensor materials and nanotechnology enhance antigen capture.
Portable devices with automated readouts reduce user error, and combining antigen detection with molecular amplification boosts accuracy. Additionally, machine learning helps interpret tricky results, ensuring more reliable detection.
These innovations aim to make RATs faster, more sensitive, and adaptable to viral mutations.
How Do Mutations in Viruses Affect RAT Detection Capabilities?
Think of viral mutations as shifting shadows in a mirror; they change the reflection, making it harder for your tests to recognize the original image.
When viruses mutate, their proteins alter, weakening the antibodies in rapid tests. This means your RATs may miss infections or give false results.
To stay ahead, you need adaptive tests with broader recognition, ensuring detection remains sharp despite the virus’s constant dance of change.
Conclusion
Imagine catching a glimpse of the invisible battle happening inside you. Rapid antigen tests shine a light on this hidden fight by quickly detecting flu and RSV proteins, guiding your next move. While they’re powerful tools, remember they’re just part of the story. By understanding their strengths and limits, you can make smarter choices. After all, in the race against viruses, knowledge is your most valuable weapon—so stay informed and stay healthy.