Photodynamic therapy (PDT) involves using light-activated drugs called photosensitizers that accumulate in cancer cells. When exposed to specific wavelengths of light, these drugs produce reactive oxygen species that damage or destroy tumors through processes like apoptosis or necrosis. PDT targets cancer cells while sparing healthy tissue, making it effective for various cancers, including skin and lung tumors. To discover how PDT can benefit you, continue exploring these innovative treatments.
Key Takeaways
- Photodynamic therapy (PDT) uses light-activated drugs called photosensitizers to produce reactive oxygen species that destroy cancer cells.
- PDT involves administering a photosensitizer that accumulates in tumors, then activating it with specific light wavelengths to induce cell death.
- The therapy can target various cancers, including skin, lung, esophageal, and head and neck tumors, with minimal damage to healthy tissue.
- Advanced light sources like lasers, LEDs, and fiber optics are used to deliver precise light doses to activate the photosensitizers.
- Emerging technologies enhance PDT effectiveness through improved photosensitizers, deeper tissue penetration, and combination with other treatments.
How Photodynamic Therapy Works at the Cellular Level

Photodynamic therapy works at the cellular level by using a photosensitizing agent that selectively accumulates in cancer cells. When exposed to a specific wavelength of light, this agent produces reactive oxygen species (ROS), which damage cellular structures and trigger cell death through apoptosis, necrosis, or autophagy.
The therapy not only targets cancer cells directly but also damages tumor blood vessels, disrupting the tumor’s blood supply and hindering its growth. The process involves the interaction between the photosensitizer, light, and oxygen, generating singlet oxygen—a highly reactive species that kills cells.
Because the light wavelength is precise, normal cells are less affected. This targeted approach allows PDT to induce oxidative stress specifically in tumor cells, leading to effective destruction with minimal harm to healthy tissue.
Types of Photosensitizers Used in Cancer Treatment

Various types of photosensitizers are employed in cancer treatment, ranging from conventional agents approved by regulatory agencies to emerging natural compounds under investigation.
Conventional photosensitizers like porfimer sodium (Photofrin) are FDA-approved and activated by red laser light. They are mainly used for esophageal and lung cancers.
Aminolevulinic acid (ALA), applied topically and activated by blue light, treats actinic keratosis and precancerous skin conditions.
Natural photosensitizers, such as plant-based compounds like curcumins, flavonoids, and alkaloids, are under study for their phototoxic and anticancer potential. These natural agents may offer fewer side effects.
Both types work by absorbing specific light wavelengths to produce reactive oxygen species, which selectively destroy cancer cells while sparing healthy tissue. Photodynamic therapy leverages these mechanisms to target malignancies effectively.
Researchers aim to optimize these agents for better efficacy in PDT. Additionally, ongoing advances in drug delivery systems are crucial for improving treatment precision and minimizing side effects.
Photoactivation mechanisms are crucial for enhancing the selectivity and effectiveness of these treatments.
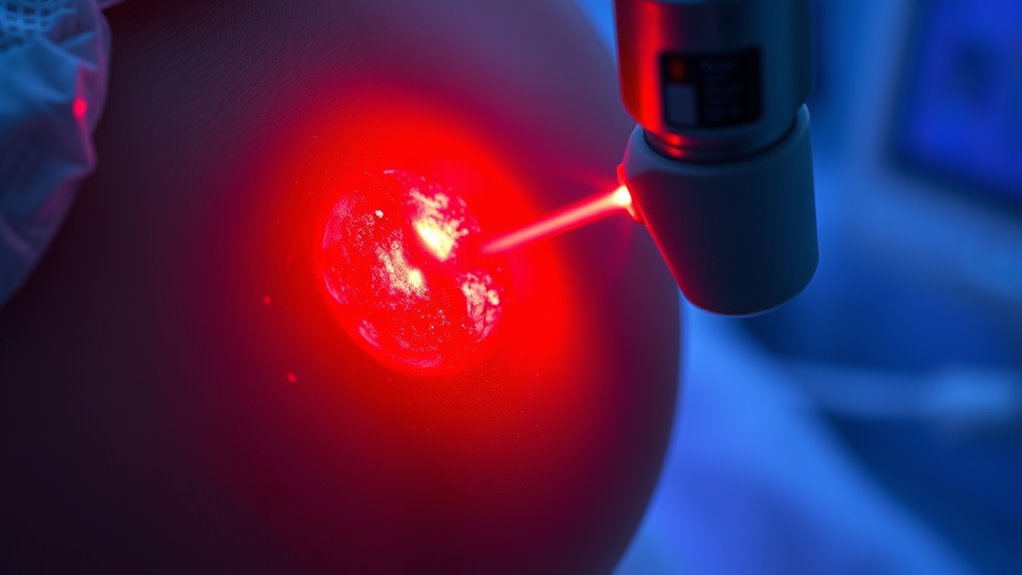
Light Sources and Delivery Methods in PDT
Different light sources play a crucial role in delivering effective photodynamic therapy (PDT), with options tailored to target tissue location and photosensitizer properties. Lasers provide high power and monochromatic light, ideal for superficial skin cancers, while LEDs offer versatility and cost-effectiveness across various treatments. Traditional lamps are less common now but still used in some cases. High refresh rates ensure consistent light delivery and treatment accuracy during procedures. Internal light sources, like chemiluminescence and bioluminescence, are being explored to improve tissue penetration in deeper areas, complemented by optical fibers that deliver light precisely to hard-to-reach spots. The choice depends on tissue depth, target size, and the specific photosensitizer’s wavelength requirements. Incorporating tissue-specific light delivery techniques can further enhance PDT efficacy for diverse clinical scenarios.
Cancers Commonly Treated With Photodynamic Therapy

Cancers treated with photodynamic therapy span a range of locations and stages, showcasing its versatility as a minimally invasive option.
For skin cancers, PDT is FDA-approved for early-stage basal cell carcinoma and squamous cell carcinoma in situ, offering effective treatment with excellent cosmetic results. Actinic keratosis, a precancerous skin condition, is commonly treated to prevent progression.
In the esophagus, Barrett’s esophagus and early-stage esophageal cancers respond well to PDT, especially for patients who can’t undergo surgery.
Lung cancers like non-small cell lung cancer benefit from PDT for localized tumors and airway obstruction relief.
Head and neck cancers, including oropharyngeal and laryngeal tumors, respond to PDT, preserving crucial structures.
Its ability to target specific tumors while sparing healthy tissue makes PDT a valuable option across these cancer types.
Administering Photosensitizers: Routes and Timing

Administering photosensitizers effectively is essential for successful photodynamic therapy, and choosing the right route depends on the tumor’s location and accessibility. Intravenous (IV) delivery is common, offering broad tissue distribution and targeted accumulation, especially for deep-seated tumors.
Effective photosensitizer delivery depends on tumor location, with IV administration being widely used for deep-seated tumors.
Topical application suits superficial skin lesions, providing localized treatment with minimal systemic exposure.
For tumors that are harder to reach, oral administration offers a non-invasive option, often used alongside fluorescence-guided surgery.
Intraperitoneal injections are being explored for advanced cancers, aiming to reduce toxicity.
Meanwhile, intratumoral injections deliver the photosensitizer directly into the tumor, minimizing off-target effects.
Understanding pharmacokinetics helps optimize timing and dosage, ensuring photosensitizers reach their peak concentration when light activation occurs, maximizing therapeutic efficacy.
Benefits and Limitations of PDT in Oncology

What makes photodynamic therapy (PDT) an attractive option in oncology is its ability to selectively target tumor cells while sparing surrounding healthy tissue. By activating photosensitizers with specific light wavelengths in the presence of oxygen, you cause direct cancer cell death and damage to tumor microvasculature, disrupting blood supply. It generates reactive oxygen species that kill cells absorbing the photosensitizer and triggers local inflammation, possibly boosting immune responses. PDT is minimally invasive, preserving organ function and offering excellent cosmetic results, especially in surface cancers. Additionally, the use of essential oils like lavender or eucalyptus has been explored for their potential to reduce inflammation and promote healing post-treatment. Furthermore, creativity can be cultivated by anyone, regardless of skill level, through consistent practice and experimentation. However, its limitations include confined treatment areas due to light penetration depth, photosensitivity reactions, and dependence on adequate oxygen levels. Technical challenges such as ensuring precise light delivery are essential for safety and effectiveness, and repeat treatments may be necessary to fully eradicate tumors.
Clinical Results and Effectiveness of Photodynamic Therapy

Clinical results demonstrate that photodynamic therapy (PDT) is highly effective in treating various skin conditions and cancers. In skin treatments, MAL-PDT achieved 84.7% full remission in actinic keratosis and 75.7% in basal cell carcinoma at three months, with high patient satisfaction (up to 90%). One-year follow-ups show no recurrence, and PDT markedly reduces acne lesions, maintaining stability or improvement. Furthermore, the vetted nature of PDT regimens ensures consistent outcomes across different clinical settings. Compared to cryotherapy, PDT offers a 14% higher chance of complete lesion clearance. For cancers like lung tumors, PDT proved feasible and safe, with tumor necrosis ranging from 5% to 50% and some complete responses. Long-term data reveal durable remission, minimal side effects, and high patient satisfaction, confirming PDT’s clinical effectiveness across dermatology and oncology. Additionally, juice cleansing practices can support overall wellness and recovery during treatment periods.
Advances in Photosensitizers and Light Technologies
Recent developments in photosensitizers (PSs) and light delivery technologies are transforming photodynamic therapy (PDT) into a more precise and effective treatment modality. Advances in molecular and nanomaterial-based PSs enhance tumor selectivity and ROS generation, especially with intelligent designs like aggregation-induced emission (AIE) and Type I PSs that produce superoxide radicals, overcoming hypoxia.
Innovations in PSs and light technologies are making PDT more precise, safe, and effective.
Near-infrared (NIR) PSs enable deeper tissue penetration and theranostic applications, although stability and targeting still need improvement.
Light technology has advanced with fiber optics, LED arrays, and two-photon excitation, allowing precise, deep, and controlled irradiation. Portable and wearable devices facilitate outpatient treatments, while integration with imaging modalities improves monitoring.
Together, these innovations remarkably increase the precision, safety, and effectiveness of PDT.
Future Perspectives and Emerging Applications of PDT

Future perspectives in photodynamic therapy (PDT) point toward expanding its applications and overcoming current limitations through innovative strategies. You’ll see efforts to combine PDT with chemotherapy, radiation, and targeted delivery methods like nanoconstructs, which enhance treatment efficacy, reduce tumor recurrence, and minimize systemic toxicity.
Advances aim to improve light penetration for treating deep tissues, using techniques like optical fibers and enhanced light sources. Researchers focus on developing more specific photosensitizers, innovative light delivery systems, and personalized protocols to optimize outcomes.
Emerging applications include treating tumors in deeper tissues, integrating PDT into multimodal therapies, and addressing drug-resistant cancers. Additionally, PDT’s potential extends to non-cancer conditions, infections, and dermatological issues, paving the way for broader, minimally invasive, and more effective treatments.
Frequently Asked Questions
Can PDT Be Used for Metastatic or Deep-Seated Tumors?
You wonder if PDT works for metastatic or deep-seated tumors. While traditionally limited to superficial tumors due to light penetration issues, recent advances aim to overcome these challenges.
You should know that combining PDT with systemic therapies and improving light delivery methods can potentially make it effective against deep or metastatic cancers. However, more clinical trials are needed to confirm its safety and efficacy for these complex cases.
What Are the Long-Term Side Effects of Photodynamic Therapy?
Long-term side effects of PDT are generally mild but can linger like a shadow. You might experience prolonged skin redness, swelling, or crusting for weeks, and pigmentation changes such as hyperpigmentation or hypopigmentation.
Photosensitivity can persist, requiring you to avoid sunlight. Rarely, scarring or skin erosion occurs.
How Does Tumor Oxygen Level Affect PDT Success?
You should know that tumor oxygen levels play a vital role in PDT success. When oxygen is abundant, ROS production increases, effectively killing cancer cells.
However, in hypoxic tumors with low oxygen, ROS generation drops, reducing treatment effectiveness. This means you need strategies to improve oxygen supply within tumors to enhance PDT outcomes, like using oxygen-delivering nanomaterials or oxygenation techniques, to guarantee better cancer cell destruction.
Is PDT Suitable for All Cancer Patients?
Imagine a spotlight shining only on the surface of a stage—if your tumor is like this illuminated area, PDT can be your spotlight, targeting superficial cancers effectively.
But if your cancer is deep in the shadows, it’s less suitable because the light can’t reach it. So, not all patients are ideal candidates; PDT works best when the cancer is localized and accessible, much like a spotlight on a stage.
Can PDT Be Combined With Other Cancer Treatments Effectively?
You might wonder if combining treatments works well. The answer is yes; combining therapies like PDT with chemotherapy, immunotherapy, or targeted drugs can boost effectiveness.
These combinations help overcome resistance, reduce side effects, and improve tumor control. By leveraging different mechanisms, you get a more extensive attack on cancer cells.
Ongoing research continues to optimize these strategies, making personalized, multimodal treatments more promising for better outcomes.
Conclusion
So, next time you’re dazzled by shiny new cancer treatments, remember photodynamic therapy—where a little light and a dash of chemicals do the dirty work. It’s like a cosmic laser show for cancer cells, minus the fireworks. Sure, it’s not perfect, but hey, who needs traditional methods when you can just turn on the lights and watch cancer fade away? Because nothing says “cutting-edge” like shining a spotlight on cancer’s demise.