Painkillers work by targeting specific molecules and nerve pathways to block or reduce pain signals. Opioids bind to receptors in your brain and spinal cord, calming pain perception. NSAIDs inhibit inflammation by blocking enzymes that produce pain-causing chemicals. Paracetamol mainly acts in the brain to lower fever and mild pain. Local anesthetics prevent nerves from firing by blocking sodium channels. To discover how these medicines compare and work in detail, keep exploring.
Key Takeaways
- Painkillers work by targeting specific receptors or enzymes involved in pain signaling and inflammation pathways.
- Opioids bind to G-protein coupled receptors (MOP, DOP, KOP) to inhibit nerve signals and reduce pain perception.
- NSAIDs block cyclooxygenase enzymes (COX-1 and COX-2), decreasing prostaglandin production that causes inflammation and pain.
- Paracetamol mainly acts in the brain by inhibiting COX-2 enzymes, lowering fever and mild pain, with minimal peripheral effects.
- Local anesthetics prevent nerve depolarization by blocking sodium channels, providing rapid, localized pain relief during procedures.
Understanding Opioids and Their Receptor Targets

Have you ever wondered how opioids relieve pain at the molecular level? When you take an opioid, it binds to specific receptors on nerve cells called G-protein coupled receptors. There are three main types: mu (MOP), delta (DOP), and kappa (KOP).
Most pain-relieving drugs like morphine target MOP receptors, which are found in your brain, spinal cord, and even in your gut. Once an opioid attaches, it activates the receptor’s internal G-proteins, leading to a chain reaction. These receptors belong to a receptor family with 7 transmembrane domains.
Most opioids like morphine target MOP receptors in the brain, spinal cord, and gut to relieve pain.
This process inhibits nerve signals by reducing neurotransmitter release and hyperpolarizing neurons. As a result, your brain perceives less pain.
These receptors play a vital role in controlling pain, mood, and even side effects like constipation through their activity in both central and peripheral nervous systems.
How NSAIDs Reduce Inflammation and Pain

Ever wondered how NSAIDs effectively reduce inflammation and alleviate pain? They work by blocking cyclooxygenase (COX) enzymes, mainly COX-1 and COX-2, which produce prostaglandins—messenger molecules that promote inflammation and pain. When NSAIDs inhibit these enzymes through competitive, reversible binding, prostaglandin production drops. This reduction decreases inflammation, swelling, redness, and heat, especially by targeting COX-2, which is linked to inflammation. NSAIDs are widely used due to their effectiveness and relatively quick onset of action. NSAIDs also lessen vasodilation, further calming inflammation. For pain relief, they inhibit prostaglandins at the injury site and may influence central nervous system pathways, interfering with neurotransmitters or NMDA receptors. This dual peripheral and central action makes NSAIDs effective for managing discomfort, while their selectivity influences their safety profile and side effects. Additionally, understanding the environmental impact of drug production can help guide safer and more sustainable medication practices.
The Role of Paracetamol in Fever and Mild Pain Relief

Paracetamol plays a central role in reducing fever and mild pain by primarily targeting the brain’s COX-2 enzymes. It inhibits prostaglandin production in the central nervous system, which helps lower body temperature and dulls pain signals. Its ability to cross the blood-brain barrier quickly, thanks to its lipid solubility, ensures rapid action in the brain. Paracetamol’s metabolite, AM404, enhances pain relief by activating pathways involved in pain and temperature regulation and indirectly modulating cannabinoid receptors. It is also considered to have a relatively favorable safety profile when used appropriately. Unlike NSAIDs, it doesn’t markedly affect peripheral inflammation, reducing side effects like stomach irritation. This central mechanism makes paracetamol effective for fever reduction and mild pain relief, providing a gentle, targeted approach that minimizes risks associated with peripheral anti-inflammatory drugs. Additionally, understanding its metabolic pathways helps in assessing safe dosages and potential interactions.
Local Anesthetics: Blocking Nerve Signals

How do local anesthetics effectively block nerve signals to produce pain relief? They work by preventing sodium ions from entering neurons, which stops the nerve from depolarizing and generating action potentials. These drugs bind to the α subunit of voltage-gated Na+ channels, locking them in their open state and blocking nerve signal transmission. To reach their target, lipophilic, un-ionized molecules cross the cell membrane and then bind inside the neuron. The pKa of each anesthetic influences its ionization, affecting how well it crosses membranes and binds to channels. Their effectiveness also depends on nerve activity; more frequent stimulation enhances their blocking ability, making them especially useful during procedures requiring rapid, localized pain relief. Understanding drug mechanisms can help in optimizing their use and minimizing side effects.
Comparing Systemic and Local Pain Relief Options
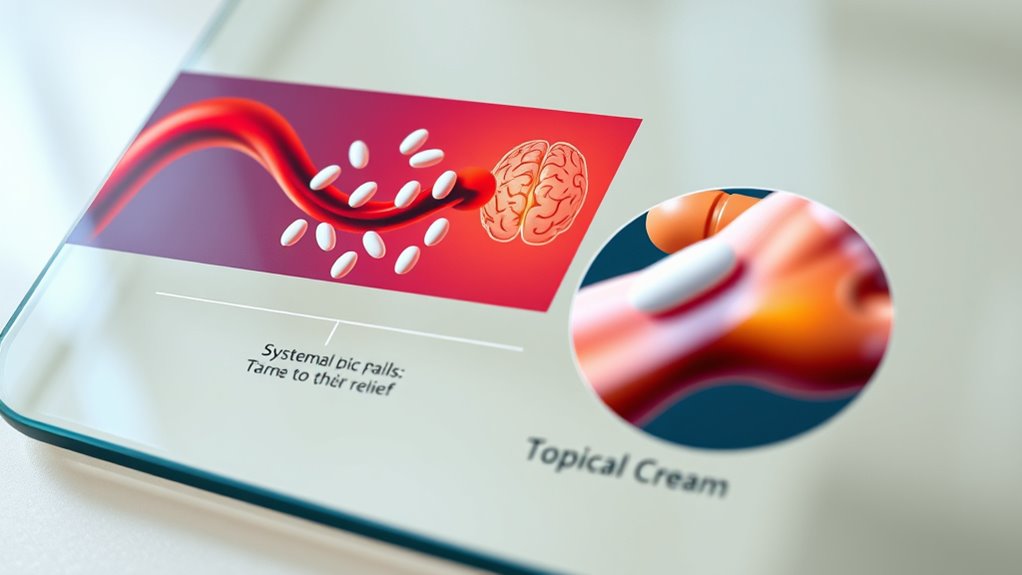
When choosing between systemic and local pain relief options, it’s important to understand how each targets pain. Systemic pain relief involves medications that affect your whole body, like NSAIDs, opioids, and paracetamol. They work by altering neural pathways and chemical mediators, making them effective for widespread pain. Forsale 100 However, they come with risks such as gastrointestinal issues or addiction. In contrast, local pain relief targets specific areas using topical NSAIDs, anesthetics, or capsaicin. They minimize systemic exposure and side effects but are less effective for large-scale pain. Local options are ideal for skin injuries or muscle strains, while systemic medications better manage extensive pain, postoperative recovery, or emergencies. Your choice depends on pain severity, location, and your health considerations.
Side Effects and Risks of Common Painkillers

Are you aware of the potential side effects and risks associated with common painkillers? Non-steroidal anti-inflammatory drugs (NSAIDs) can cause headaches, stomach pain, nausea, diarrhea, and dizziness.
Long-term or high-dose use may lead to stomach ulcers, internal bleeding, and anemia. They can also trigger allergic reactions like rashes and sensitivity to sunlight.
Risks increase with prolonged use, especially for heart problems such as heart attacks, strokes, or heart failure, and they can impair kidney and liver functions. Essential oils, for example, are natural alternatives that may support pain relief without the same risks, though they should be used appropriately.
Opioid painkillers often cause nausea, constipation, dizziness, dry mouth, and itching. They may also slow breathing and cause drowsiness.
Long-term use of opioids risks dependence and addiction.
Combining painkillers or using them with blood thinners raises additional bleeding concerns.
Always monitor for adverse effects and consult your healthcare provider.
The Chemistry Behind Painkiller Action

Ever wonder what makes painkillers effective at reducing pain and inflammation? It all comes down to their chemistry. NSAIDs work by blocking cyclo-oxygenase (COX) enzymes—mainly COX-1 and COX-2—that produce prostaglandins. These lipid compounds promote inflammation, pain, and fever by sensitizing nerve endings. When you take an NSAID, it reversibly inhibits COX enzymes, reducing prostaglandin synthesis and calming inflammation. Paracetamol, on the other hand, acts mainly in the brain, likely inhibiting a brain-specific COX variant to decrease pain and fever, and possibly influencing serotonin pathways. Opioids bind to mu-opioid receptors in the nervous system, inhibiting pain signal transmission and releasing dopamine, which creates pain relief and euphoria. This chemistry allows painkillers to target different parts of the pain pathway effectively. Understanding how these enzyme inhibitors work helps us appreciate the precise ways medicines can modulate our body’s response to pain.
Choosing the Right Pain Relief for Different Needs

Choosing the right pain relief depends on understanding your specific pain characteristics and needs. First, identify the type—acute, chronic, or inflammatory—as each responds differently.
For mild pain, over-the-counter options like acetaminophen work well, while severe pain may require stronger NSAIDs or prescription medications.
Consider the location; topical treatments are effective for localized pain, whereas widespread pain often needs oral drugs.
Think about how long you’ve experienced the pain—chronic issues often need tailored, ongoing strategies.
Also, evaluate how pain impacts your daily life. If inflammation is involved, NSAIDs are helpful, but they can cause stomach issues.
Always factor in your medical conditions, allergies, age, and pregnancy status.
Consulting a healthcare professional ensures you choose the safest, most effective option for your needs.
Understanding home organization principles can also help manage the environment that might influence your overall comfort and well-being.
Frequently Asked Questions
How Do Opioids Affect Mood and Consciousness?
You might notice opioids impact your mood by increasing dopamine, making you feel more positive and less distressed. They also alter brain activity in areas linked to emotions, reducing negative responses and boosting positive ones.
Consciousness can be affected too, causing changes in sleep and wakefulness, sometimes leading to disorientation. These effects happen because opioids activate specific receptors, influencing neurotransmitter release and neural circuits involved in mood and awareness.
Can NSAIDS Be Used Long-Term Safely?
You’re wondering if NSAIDs can be used safely long-term. While they’re effective for pain relief, prolonged use increases your risk of gastrointestinal, cardiovascular, and kidney problems.
To use NSAIDs safely, you should take the lowest dose for the shortest time, monitor your health regularly, and consult your healthcare provider.
Consider alternatives like acetaminophen or non-pharmacological therapies, especially if you have pre-existing health conditions or are at higher risk.
Why Does Paracetamol Have Fewer Side Effects Than NSAIDS?
Imagine walking through a garden without weeds. Paracetamol, like a gentle gardener, targets pain signals in your brain, causing fewer side effects.
Unlike NSAIDs, it doesn’t reduce inflammation or irritate your stomach lining. This focused action means you experience milder effects, mainly avoiding risks like stomach ulcers or kidney issues.
How Quickly Do Local Anesthetics Take Effect?
You want to know how quickly local anesthetics work. Usually, they start acting within 1 to 2 minutes after infiltration or topical application.
The onset depends on factors like the route of administration, with superficial methods acting faster, and the type of anesthetic used; shorter-acting agents act sooner.
Conditions such as tissue pH, blood flow, and additives like bicarbonate can also influence how quickly they take effect.
What Determines the Choice Between Systemic and Topical Painkillers?
You weigh the depth and reach of your pain—like deciding between a broad landscape or a specific point. If your pain is widespread or deep, you opt for systemic painkillers to cover more ground quickly.
For localized discomfort, topical options target the pain site directly, minimizing side effects. Your choice hinges on pain location, severity, safety concerns, and personal preferences, helping you manage pain effectively with fewer risks.
Conclusion
Now that you know how painkillers work, you hold the keys to steering your relief options like a skilled navigator steering through stormy seas. Whether it’s the gentle whisper of paracetamol or the powerful embrace of opioids, understanding their chemistry helps you choose wisely. Think of painkillers as allies in your journey, each with unique strengths and shadows. With this knowledge, you can chart a course toward comfort, steering clear of storms and into calmer waters.